"Frozen shoulder" - myths, truths and treatments. Part 2
This is the second of a 2 part series. Click here for Part 1.
We know that this can be incredibly painful and debilitating, with inflammation, changes in important shoulder structures and nasty suffering.
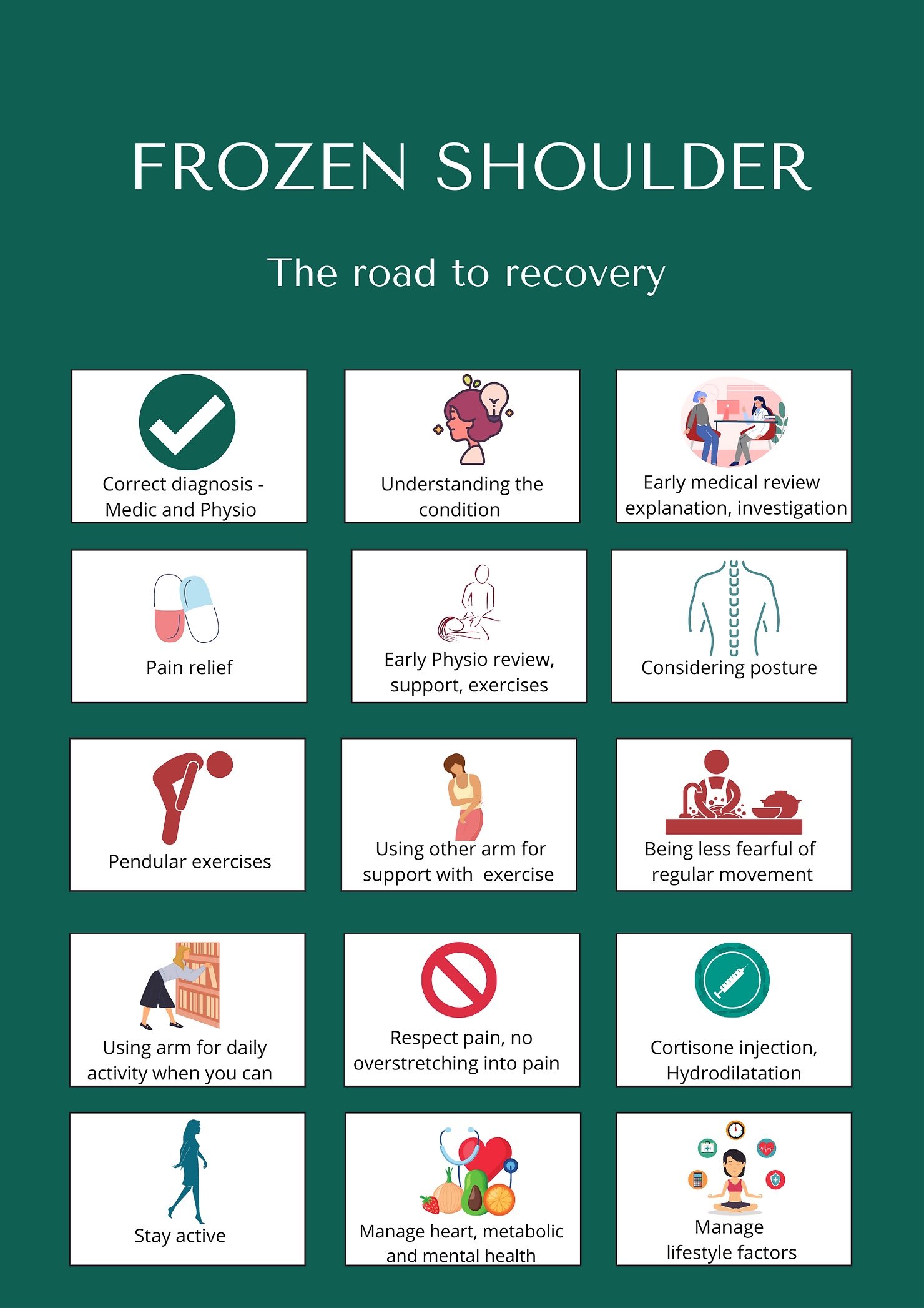
So how do you manage it yourself, or get the right help? There is no 'one size fits all approach', but there are basic principles to follow and steps to recovery.
'Wait and see' vs the latest treatments
In the past, it's been said that a 'wait and see' approach, with minimal Physio, was best, based on a quasi-experimental, biased studies. We now know that we should offer deserving patients far more. Current treatment pathways, including NHS pathways, recommend ongoing Physio support alongside xrays, education, health screening and, if necessary, steroid injections and hydrodilatation (Lewis, 2015, Rangan, 2020).
Frozen shoulder: the 10 step process
These steps are based on the latest research, including recent UK FROST study, the largest randomised trial comparing common treatments, including Physio and steroid injections.
1) Get the right diagnosis early. Get this wrong and you'll get the treatment wrong too. Pain and stiffness will fluctuate, and it may last months or years, but you can influence this timeline by following advice and getting seen early.
2) Understand the condition. Your doctor and Physio can help with this, using models and blogs like this to help. The more you know, the more empowered you will be, but be sure to get the info from those you can trust. For the truly geeky and health care professionals who want a scientific understanding of frozen shoulder, see here.
Understanding the condition will make you feel in control, manage pain and get the best treatment.
3) See the doctor. It's lovely to get tips and empathy from neighbours and friends, but your GP, Physio and Medical Consultants understand the pathology. They can correctly diagnose the problem, rule out other causes, can order scans, and guide you on best management
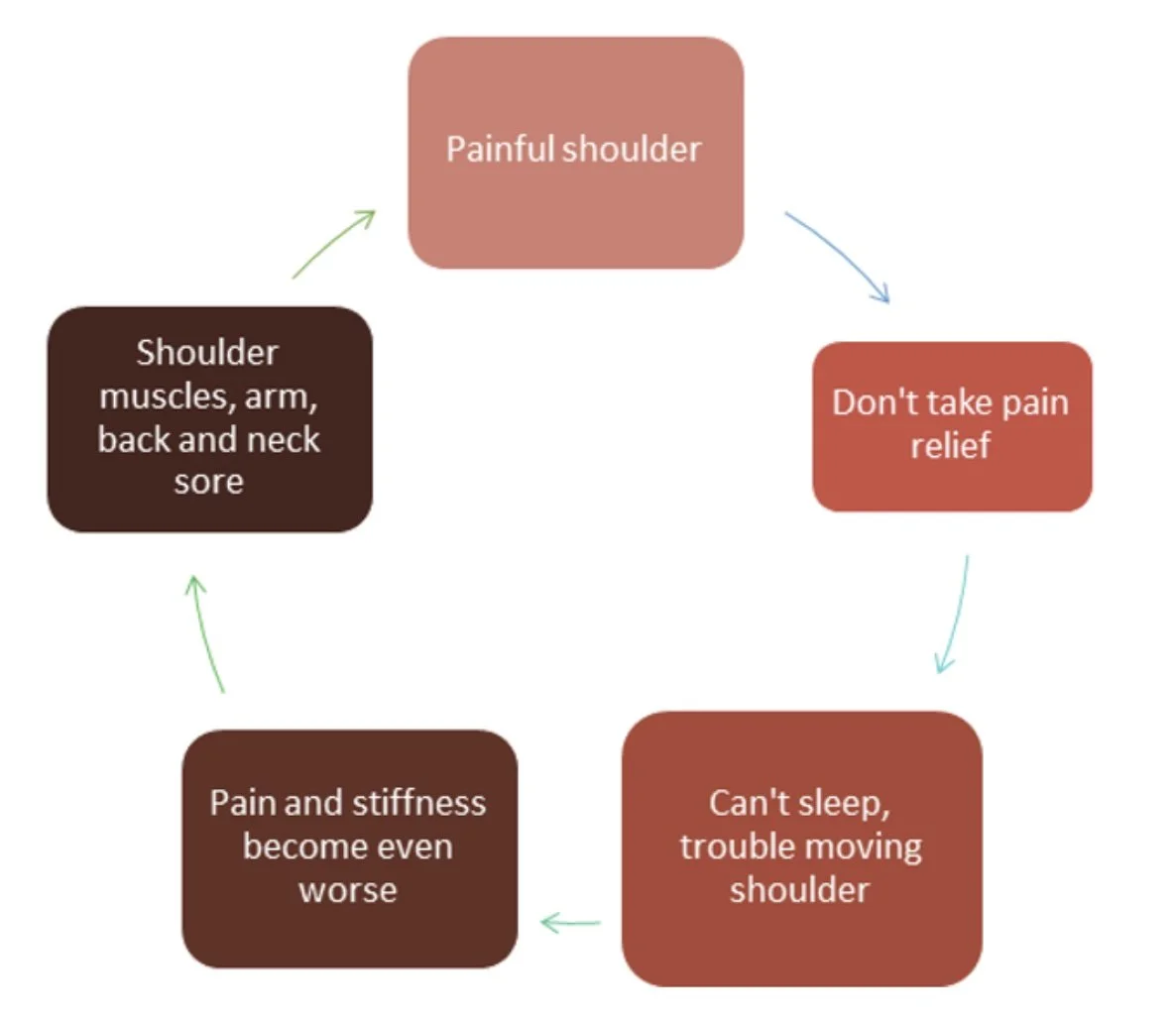
4) Use pain relief if necessary. Pain relief is a vital part of making life tolerable and improving movement, not to mention getting sleep! People are, understandably, often reluctant to take pain killers, not wanting to 'mask the pain' or rely on drugs. The truth is that by not taking pain relief, you can end up in a cycle of pain, making it even worse. Short term pain relief lets you to move the shoulder. This promotes blood flow and normal movement.
4) See the Physio. Physios can help with diagnosis if it's unclear. They can see you face to face, formal tests and time to review you (unlike some GPs) which makes diagnosis easier and often, more accurate. They will explain what's going on and guide you towards the right resources. Once you have a diagnosis, you should have both Medical and Physio care. As well as giving you exercises, advice and possibly manual therapy, Physios can provide an understanding of the condition, an empathetic ear and guidance on treatment options.
Gentle, assisted movement and prescribed exercises can help.
5) Be mindful of posture. If you're in pain, you'll hold yourself awkwardly and often cradle the arm. Check your shoulder and arm position in the mirror. Try and hold it as normally as possible.
6) Try gentle exercises, move the arm when you can. Pendular exercises - literally moving your arm like a pendulum - and gentle supported movement are recommended, but I'd advise against just getting exercises from the internet or a generic frozen shoulder handout . Generic exercises don't account for your unique circumstances, and what is often a combination of a 'frozen shoulder' and other problems, like rotator cuff inflammation and referred pain. You could do more harm than good. Use the opposite arm for support with exercise and regular movement if necessary. Frozen shoulder is more common in the non dominant arm as we tend to use it less, so it makes sense to use the other arm when we can to get things gently moving and reduce pain. You don't want the pain to escalate as a result of exercises! If you are in pain at rest, it might be a little worse with movement, but that should be mild and momentary. If pain is anything more than mildly worse during an exercise or causes more pain after the exercise, stop. Your Physio can show you specialised supported exercises so you can move without aggravating the problem.
7) Don't overstretch into pain. Avoid putting your hand above or to the side of you on a doorway and stretching or pulling, it will make things worse. Manage expectations too - a medical and physio treatment plan will help you to balance what you can and can't do and set realistic goals.
8) Cortisone injections really can help some patients. A combination of saline, steroid and an anaesthetic, Cortisone injections will dampen the inflammation, and it's possibly better to have it sooner rather than later.
9). Hydrodilatation is the latest treatment trend. It involves an injection of saline, anaesthetic and steroid, under the Xray or ultrasound guidance. This opens up the joint and releases contracted tissue and adhesions. For reliable information and videos on the procedure, see here.
So how do you decide if cortisone injections or hydrodilatation are right for you? If you are not sleeping much and really struggling with pain, evidence shows they can really help. It's a personal decision, best discussed with your health care professionals. If you have these medical procedures, take it easy for the first week or so afterwards for the treatment to have its full effects. You may have some immediate relief from pain and stiffness, but it can take 6 weeks for the full benefits to appear, so be patient. Be aware that effects can be significant, but also shortlived.
When to have these procedures? It seems timing matters - earlier is probably better. Some research indicates that it might help change the trajectory of the condition if given early enough, reducing inflammation overall and the time it takes to resolve.
10) Manage your health, control what you can. We know frozen shoulder involves inflammation and is associated with conditions like diabetes and thyroid problems. It's also clear inactivity predisposes us to it and stress makes it worse. Managing wider health will help you cope mentally and may help the condition, whilst just walking and breaks from sitting will get the arm gently moving.
Hopefully this sensible yet scientific approach will help you on your way and reassure you that you don't have to face this alone.
References
Challoumas et al. Comparison of treatments for a Frozen Shoulder: A systematic review and meta-analysis. JAMA 2020 Dec 1;3(12) DOI: 10.1001/jamanetworkopen.2020.29581.
Cucci, D. et al. Risk factors for shoulder stiffness: current concepts. Joints. 2017 Dec 11;5(4):217-223. DOI: 10.1055/s-0037-1608951
De Baets et al. Are clinical outcomes of frozen shoulder linked to pain, structural factors or pain related cognitions? An explorative cohort study. Musculoskelet Sci Pract 2020. Dec:0:102270. DOI: 10.1016/j.msksp.2020.102270
Kingston, K. et al. Shoulder adhesive capsulitis: epidemiology and predictors of surgery. J Shoulder Elbow Surg 2018 Aug;27(8):1437-1443. DOI: 10.1016/j.jse.2018.04.004
Lewis, J. Masterclass: Frozen shoulder contracture syndrome - aetiology, diagnosis and management. Manual Therapy 2015: Volume 20, Issue 1, pages 2-9. DOI: https://doi.org/10.1016/j.math.2014.07.006
Lluch-Girbes, E. et al. A central nervous system-focused treatment approach for people with frozen shoulder: protocol for a randomised controlled trial. Trials. 2019 Aug 13;20(1):498. DOI: 10.1186/s13063-019-3585-z
Rangan, A. et al. Management of adults with primary frozen shoulder in secondary care (UK FROST): a multicentre, pragmatic, three-arm, superiority randomised clinical trial. The Lancet, Oct 2020: Vol. 396, Issue 10256, 977 - 989. DOI: https://doi.org/10.1016/S0140-6736(20)31965-6